
By: Destiny Howard, MS, RDN, LD
Doctors talk about it and articles mention it, but what exactly is insulin resistance, and why does it feel like such a mystery?
We’re going to break down what insulin resistance is (and why the mainstream low-carb approach isn’t the best solution).
Insulin is a hormone produced by the pancreas that helps glucose enter the cells in your body so you can use it for energy. Imagine insulin as the key that unlocks the doors of your body’s cells to let glucose in.
When you eat foods, especially carbohydrate foods (like bread, pasta, fruits, and starch vegetables), your body “digests” them, breaking them down into sugar (a.k.a. glucose). The glucose is absorbed by your gut and enters your blood.
Glucose is the main form of energy that the cells in your body need to do all of the important things they do, like help you breathe and think and walk! But here’s the catch: sugar can’t just waltz right into your cells all on its own. There’s a lock on the door to keep other things from getting inside. It needs insulin to act as the key, unlocking the cell’s “doors” for glucose to enter.
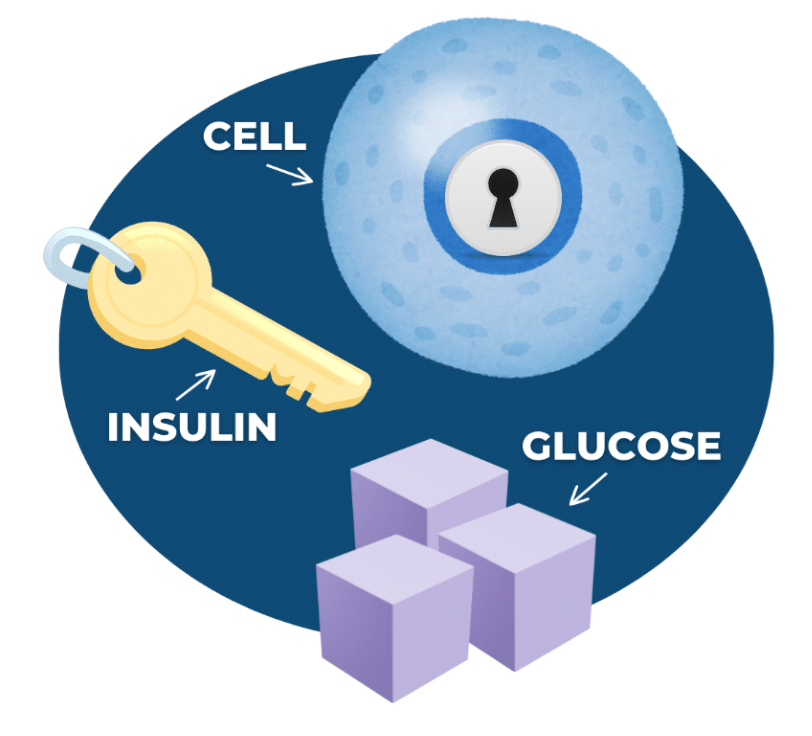
So, when you eat, your blood sugar levels rise, and your pancreas releases insulin into your blood. Insulin then travels through your body and acts as a key that opens up the door of your cells to let the glucose in.
When cells become “insulin resistant,” it means they don’t respond to insulin as well or as quickly as they should. It’s almost like the locks on the cell doors are rusty, or jammed. Even though you have the key (insulin), it takes more time and effort to open the door. Meanwhile, glucose is stuck waiting outside.
1. All the glucose “waiting in line” signals the pancreas to make and release more insulin. That’s why insulin levels increase–an early sign of insulin resistance.
2. The glucose level in your bloodstream gets higher because it has nowhere else to go. This is how insulin resistance eventually leads to high blood sugar levels.
3. The cell starts to run out of “fuel,” because even though glucose is nearby, it can’t be used for energy from the outside! This can cause fatigue and hunger, especially for foods that contain carbs. Your cells can be “hungry” for energy (a.k.a. glucose), even if you JUST ate.
Because there are SO many factors that play into it, we don’t yet know the specific reasons a person develops insulin resistance. However, we DO know some ways to help our cells respond to insulin, or “grease the lock,” so to speak.
You might be thinking, “I know, I know, I need to eat less carbs…” But what if we told you that the mainstream approach of cutting carbs isn’t all it’s cracked up to be?
People often believe that low-carb diets are effective long-term for insulin resistance for a few reasons. One reason is based on the theory that with less carbohydrates to process, there will be less glucose and the body will need less insulin to manage blood sugar levels. This can reduce the workload on the pancreas, improving insulin sensitivity over time. While this is true, it’s not the whole story!
Cutting carbs might seem like a quick fix for managing insulin resistance, but it’s not the only solution, and it may not be the best solution long-term.
Here are three ways low-carb diets totally miss the mark when it comes to long-term results and why we, as registered dietitians who specialize in digestive health and eating disorders, take a different approach.
Glucose, from carbohydrates, is the preferred source of energy for our bodies, particularly our brain and our muscles.
Foods like breads, pastas, fruits, and starchy vegetables also provide essential vitamins and minerals that are vital for health as well as phytonutrients that help reduce inflammation. (Psst…we’re talking about the same inflammation that’s been linked to insulin resistance. Interesting…).
In practice, we’ve seen people who restrict in such a way that they develop nutrient deficiencies and metabolic changes that make insulin resistance worse.
Additionally, carbohydrates serve as a key source of fiber, which supports digestive health, promotes feelings of fullness and satiety, and helps regulate blood sugar levels.
The short of it is, carbs are certainly not “bad” for you, even if you have insulin resistance. And why miss out on beneficial nutrients if you don’t have to?
Something that isn’t talked about enough in the health and wellness space is how low-carb diets can backfire, leading to weight cycling and binge eating, both of which have negative effects on insulin resistance.
People who restrict carbohydrates may experience rapid initial weight loss, often due to water weight loss from muscle glycogen depletion. This weight loss is usually not sustainable. In fact, evidence suggests that 95% of people will regain the weight that they lost, if not more. This cycle of weight loss and regain, known as weight cycling, places significant stress on the body. It can disrupt hormonal balance, reduce metabolic rate, and increase inflammation. Yikes.
Beyond that, the strict rules and limits of low-carb diets contribute to feeling deprived or anxious around food, increasing the likelihood of binge eating. After a while, a person may feel out of control and have episodes of uncontrollable overeating (often on high-carbohydrate foods). This vicious cycle of restriction and binge eating may result in feelings of guilt, shame, and worsen disordered eating patterns. It’s unhelpful, to say the least.
Truth be told, major mental health challenges can come from low-carb diets. It’s a big reason why the long-term effectiveness for managing insulin resistance is up for debate.
Some low-carb dieters experience side effects like mood changes, fatigue, and brain fog. This is because carbohydrates play a role in the production of serotonin, a neurotransmitter that regulates mood. Drastically reducing your carb intake can lead to fluctuations in serotonin levels, potentially resulting in irritability or feelings of depression.
Individuals on low-carb diets also experience challenges when dining out, attending social gatherings, or sharing meals with family and friends. The restrictive nature of these diets can limit food choices and make it difficult to eat in social settings. They may feel isolated, frustrated, or excluded from social activities centered around food.
Furthermore, the emphasis on weight loss in popular low-carb diet culture can provoke disordered eating behaviors and fuel preoccupations with food and weight. These behaviors, unfortunately, increase the risk for developing or relapsing an eating disorder.
So, what’s the alternative? Rather than cutting carbs out of your life, you can add beneficial foods to your diet and practice kindness toward your body. It’s time to focus on your overall well-being so you can have lasting results!
We’ve put together a free digital download that includes 4 simple (yet effective) nutrition strategies and 4 lifestyle strategies for insulin resistance. No strings attached!
…Okay, just one string. We want to add you to our email list so you can get to know us better and learn about other free resources in our newsletter! Click here to access.
Our dietitians work 1:1 with clients, offering personalized support for managing insulin resistance through an eating disorder-informed, weight-inclusive, non-diet approach. We help people create custom plans that cater to their lifestyle, health needs, and the foods they love to eat. If you’re interested in working with us, click here to join our waiting list.

We are a group of dietitian specialists based in Oklahoma offering virtual nutrition therapy for digestive health and disordered eating recovery.
We love working with individuals who are ready to find relief from gastrointestinal (GI) symptoms and embrace a more positive relationship with food and their bodies.
Offering virtual nutrition counseling services in Oklahoma, Texas, West Virginia, and other select states.